|
|
|
| Relationship Between Periodontitis And Anemia - Does It Exist? |
Gayatri 1 , Maima Rani Ishwary 2 , Anirban Chaterjee 3 , Ahad M Hussain 4 , Praveen J 5 , Deepika J 6
1 Professor , Dept. of Periodontics - The Oxford Dental College
2 Post Graduate Student , Dept. of Periodontics - The Oxford Dental College
3 Professor And Head Of Department , Dept. of Periodontics - The Oxford Dental College
4 Reader , Dept. of Periodontics - The Oxford Dental College
5 Reader , Dept. of Periodontics - The Oxford Dental College
6 Senior Lecturer , Dept. of Periodontics - The Oxford Dental College
|
| Address For Correspondence |
Dr. Gayatri Gundannavar
The Oxford Dental College And Hospital
10th Mile, Bommanahalli
Hosur Road, Bangalore 5600068 |
| Abstract |
| Aims: To evaluate the relationship between periodontitis and anemia.
Methods and material: 30 patients, 15 with gingivitis and 15 with chronic periodontitis participated in this study. Plaque index, bleeding on probing, pocket depth were recorded for the patients. A complete hemogram including Hb%, RBC count, ESR, PVC, MCHC, MCV, etc. were recorded. The patients were subjected to scaling and root planning. The clinical parameters were compared to the hematologic parameters in both the groups.
Results: The clinical parameters did not correlate with the haematological parameters in both the groups.
Conclusions: This study shows that periodontal disease and anaemia may not be related, and the occurrence of them may be independent of each other. |
|
| Keywords |
| Anaemia and periodontitis. |
|
| Full Text |
Introduction:
Periodontitis is an inflammatory disease of the supporting tissues of the tooth which is caused by specific microorganisms in a susceptible host. The bacteria and their product provoke an inflammatory reaction to the host tissues. The ulcerated pocket epithelium around the affected teeth form a ‘porte d entre’ for bacteria and their products such as endotoxins.[1] Bacteraemia in periodontitis has been demonstrated and the extent is directly related to the severity of the inflammation of the periodontal disease. Subgingival microflora in patients with periodontitis causes a significant and persistent bacterial challenge to the host. Several research group have demonstrated that periodontitis is associated with elevated number of WBC[2],[3], C-reactive protein[4], IL6[5], eryththrocytes[6] etc. It has therefore been speculated that periodontitis results in a low grade systemic infection.
Anaemia of Chronic Disease (ACD) is defined as anaemia occurring in chronic infection, chronic inflammatory process or tumour formation that is not due to dysfunction of bone marrow cells or other disease, and occurring despite of adequate iron stores and vitamins.[7],[8],[9] A Characteristic finding of the disorder associated with ACD is increased production of cytokines that mediate inflammatory response such as TNF, IL1 and interferone. All the process involved in the development of ACD can be attributed to these cytokines including shortened RBC survival, blunted erythropoietic response to anaemia, impaired erythroid colony formation and abnormal mobilization of reticuloendothelial iron stores.[10]
These cytokines are also released by periodontitis tissues in response to bacterial infection which suggests that periodontitis like other chronic diseases may cause ACD.
Therefore the aim of the present study was to investigate the association between haematological parameters and clinical parameters in patients with chronic gingivitis and periodontitis.
Materials and methods:
Source of data: Subjects visiting the Department of Periodontics The Oxford Dental College and Hospital, Bommanahalli, Hosur road Bangalore, The purpose of the study was explained to the subjects and an informed consent was obtained from all the subjects prior to the study.
Method of collection of data:
Sample size: total 30 subjects (both male and female) were included in the study.
Subjects were divided into 2 groups
Group A patients (n=15) which includes patients with chronic generalised gingivitis.
Group B patients (n=15) which includes patients with chronic periodontitis.
Inclusion criteria:
Group A: comprised of 15 systemically healthy adult patients aged 20 to 55 years showing clinical signs of gingivitis (reddening, loss of stippling, bleeding on probing) with no signs of periodontitis.
Group B: was comprised of 15 systemically healthy adult patients aged 20 to 55 years diagnosed clinically and radiographically as chronic periodontitis with gingival inflammation, pocket depths greater than 5 mm, clinical attachment loss of more than 3mm in more than 20 teeth with moderate to severe bone loss. Chronic periodontitis will be diagnosed based on the criteria of American Academy of Periodontology classification of periodontal diseases 1999.
Exclusion criteria:
1. Patients with history of systemic disorders.
2. Patients on antibiotics in the past 6 months.
3. Patient with current or past habit of tobacco smoking or chewing.
4. Patients with history of periodontal disease in the previous 6 months.
Clinical Parameters recorded:
1. Plaque index.[11]
2. Bleeding on probing.
3. Probing pocket depth.
4. Clinical attachment level.
Study Design:
A detailed case history and the above mentioned clinical parameters were recorded for each patient. Venous blood samples were obtained by veini puncture in the antecubital fossa. The blood samples were collected in EDTA bulband and processed within 4 hours of collection in an automated haematology analyser. The laboratory blood investigations included haemoglobin (Hb %), total number of erythrocytes, pack cell volume, erythrocyte sedimentation rate, mean corpuscular volume of erythrocytes and mean corpuscular haemoglobin concentration.
Statistical Analysis
Statistical test used: t- test/Mann-Whitney test
Decision Criterion: We compare the P-Value with the level of significance. If P<0.05, we reject the null hypothesis and accept the alternate hypothesis. If P>0.05, we accept the null hypothesis.
Results:
The study sample consisted of 18 males and 12 females. The mean age for the gingivitis group was 34.27 years and for the periodontitis group was 41.40 years.
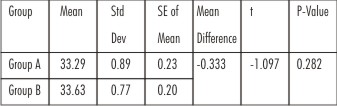
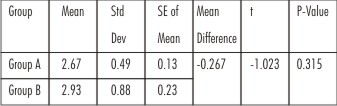
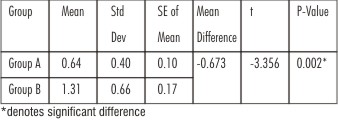
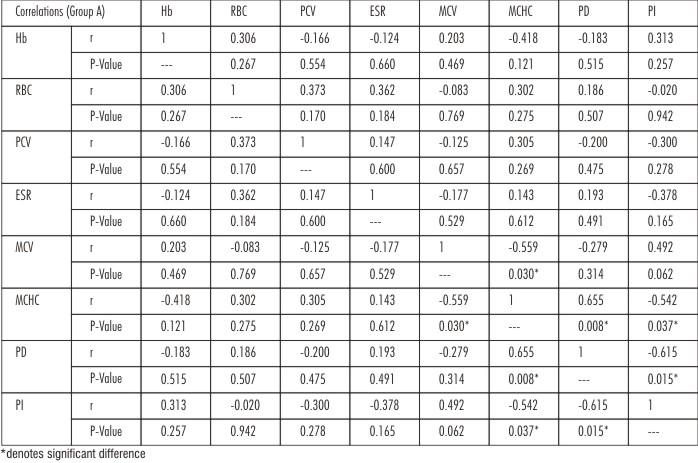
Slightly higher mean haemoglobin percentage was recorded in group B (13.45%) as compared to group A (13.02%), but the difference between them was not statistically significant (Table 1). The RBC count in group A was 4.64 million/dl, this was slightly higher than the RBC count of group B (4.59 million/dl). The difference between the two groups was not statistically significant (Table 2). The pack cell volume recorded in group A was slightly higher when compared to group B but the difference between them was not statistically significant (Table 3). Higher mean ESR was recorded in group B compared to group A and the difference between them was not statistically significant (Table 4). Higher MCV value was recorded for group A when compared to group B and the difference between them was not statistically significant (Table 5) and slightly higher MCHC value was recorded for group B when compared to group A and the difference between them was not statistically significant (Table 6). Bleeding on probing was present in both the groups, the probing depths and the plaque index were slightly higher in group B as compared to group A but this was not statistically significant (Table 7). Group B had a higher plaque index score which was of statistical significance (Table 10). The clinical attachment level was only recorded in group B, the mean of which was 3.25 mm suggesting that Group B had a moderate form of periodontitis (Table 8). There was a slight negative correlation of haemoglobin and MCV to probing depth in group A. There was a slight positive correlation of MCHC to probing depth in group A. The haemoglobin and the MCV positively correlated to the plaque index in group A and whereas the MCHC negatively correlated with the plaque index in group A. All these correlations were not of any statistical significance (Table 11,Graph 1). For group B the haemoglobin %, pack cell volume and MCV had a negative correlation to probing depth whereas the MCHC had a positive correlation to probing depth. The haemoglobin, PCV and MCV had a positive correlation to plaque index and MCHC had a negative correlation to plaque index in group B and all these correlations were not of statistical significance (Table 12,Graph 2).
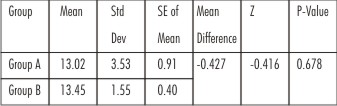 | Table 1 - Comparison Of Hb Between The Groups (Mann-Whitney test)
 |
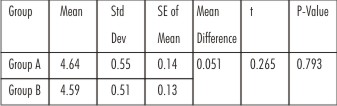 | Table 2 - Comparison Of Rbc Between The Groups (t- test)
 |
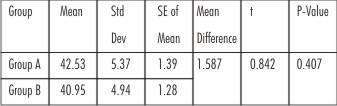 | Table 3 - Comparison Of Pcv Between The Groups (t- test)
 |
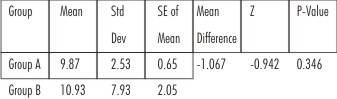 | Table 4 - Comparison Of Esr Between The Groups (Mann-Whitney test)
 |
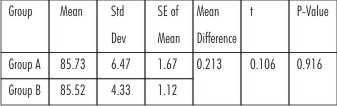 | Table 5 - Comparison Of Mcv Between The Groups (t- test)
 |
 | Table 6 - Comparison Of Mchc Between The Groups (t- test)
 |
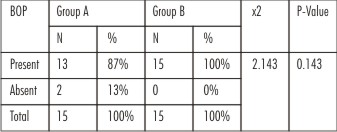 | Table 7 - Bop In The Two Groups
 |
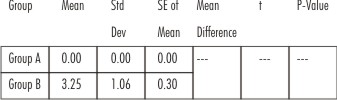 | Table 8 - Cal Comparison Between The Two Groups
 |
 | Table 9 - Pd Comparison Between The Two Groups
 |
 | Table 10 - Pi Comparison Between The Two Groups
 |
 | Table 11 - Correlation Between Different Parameters In Group A
 |
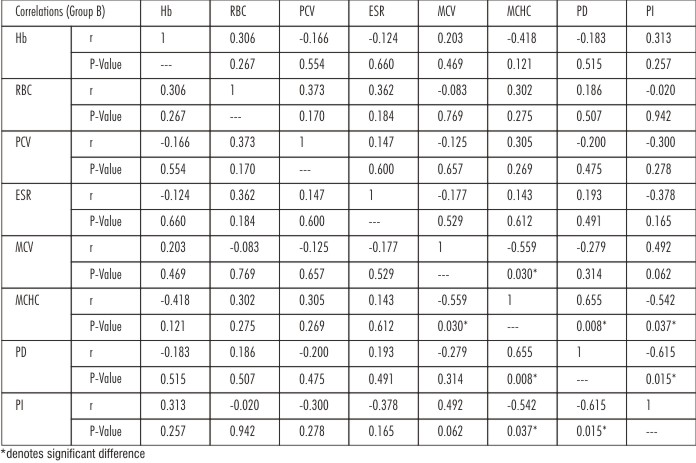 | Table 12 - Correlation Between Different Parameters In Group B
 |
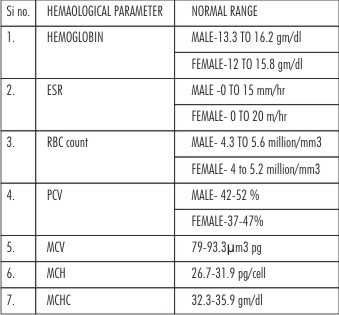 | Table 13 - Reference Values For Laboratory Tests
 |
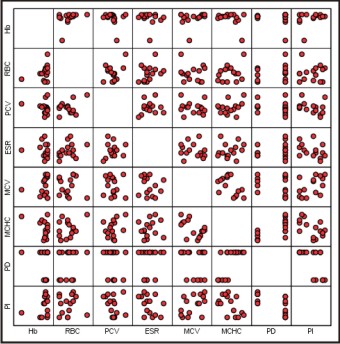 | Graph 1 - Scatter Plot – Group A: (Correlation Graph)
 |
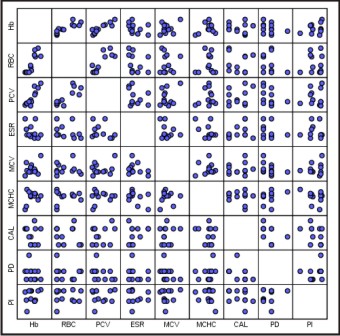 | Graph 2 - Scatter Plot – Group B: (Correlation Graph)
 |
Discussion:
The aim of the present study was to investigate the haematological status of patients with gingivitis and periodontitis.
The concept of periodontal disease as a localised entity affecting only the teeth and the supporting apparatus has been revised as it has been seen that rather than being confined to the periodontium periodontal disease has a wide range of systemic effects. Periodontal disease has a proven relationship with several systemic conditions like cardio vascular disease, diabetes mellitus, adverse pregnancy outcome, obesity and stroke.[12],[13],[14],[15],[16] One of the lesser documented associations has been interrelationship between periodontal disease and anaemia.
Anaemia of chronic disease is an immune driven process in which cytokines result in decreased erythropoietin production, impaired proliferation of erythroid progenitor cells and disturbed iron haemostasis. This normocytic and normochromic anaemia has been described in many chronic diseases like rheumatoid arthritis, renal failure, bacterial and parasitic infections etc.[17],[18]
The association of anaemia and periodontitis has been explored since the early 20th century. Earlier reports have suggested anaemia to be a cause and not a consequence of destructive periodontitis. Lainson et al.[19] was one of the first authors to implicate anaemia as a systemic cause of periodontitis. Hutter et al.[20] and Thomas et al.[21] found that periodontitis patients had lower hematocrit, lower erythrocytes, lower haemoglobin % and higher ESR when compared to healthy controls.
In our study the periodontitis group had a higher haemoglobin %, MCHC and ESR as compared to the gingivitis group. On the other hand PCV, MCV and RBC count was found to be higher in the gingivitis group as compared to the periodontitis group. The difference between the two groups was not of statistical significance. Also the values for all the haematological parameters were well within the normal range.[22]
The probing depth, plaque index and bleeding on probing were higher in the periodontitis group as expected. Since clinical attachment loss was absent in the gingivitis group no statistical comparison was possible. But the average clinical attachment level for the periodontitis group was 3.25 mm indicating it to be moderate periodontitis.
The increase haemoglobin % found in our study has also been reported by Wakai et al.[23] who found higher haemoglobin % levels in patients with higher CPITN scores. Aljohani H [24] and Havemose Paulsen A[25] also have reported increased heamoglobin % with increased severity of periodontitis. The periodontitis group in our study was of a mild to moderate nature whereas most of the studies which showed correlation between anaemia and periodontitis had patients with severe periodontitis. In another study by Enhos S et al.[26] found no correlation between anaemia and periodontitis.
Chronic periodontitis is a milder inflammatory condition compared to other systemic infections or conditions like rheumatoid arthritis, neoplastic conditions and fungal or parasitic infections. Hence it may not be enough to show drastic haematological status in periodontitis patients.[27]
Conclusion:
Based on the results obtained from the study we can conclude that there is no correlation between anaemia and periodontitis. The occurrence of the two may be independent of each other. These results could have been different if our study had a larger sample size and recruited patients with severe periodontitis.
References:
1. Scannapicco F A, Bush R B, Paju S. Associations between periodontal disease and risk factors for atherosclerosis, cardiovascular diseases and stroke. A systematic review. Ann Periodontal 200;8:38-53.
2. Kweider M, Lowe G D, Murray G D, Kinane D F, McGowan B A. Dental disease, fibrinogen and white cell count links with myocardial infarction? Scott Med J 1993;38(3):73-74.
3. Christan C, Dietrich T, Hagewald S, Kage A, Berniemoutin J P. white blood cell count in generalised aggressive periodontitis after non surgical periodontal therapy. J Clin Periodontol 2002:29(3):201-206.
4. Noack B, Jenco R J, Trevisan M, Grossi S, Zambon J J, De Nardin E. Periodontal infections contribute to elevated systemic C reactive protein level. J Periodontol 2001;72(9):1221-1227.
5. Mengel R, Bacher M, Flores De Jacob L. Interactions between stress, interleukin 1 β, interleukin 6 and cortisol in periodontally diseased patients. J Clin Periodontol 2002;29(4):1012-1022.
6. Salvi G E, Lawrence H P, Offenbacher S, Beck J D. Influence of risk factors on pathogenesis of periodontitis. Periodontol 2000 1997;14:173-201.
7. Lee G R. The anaemia of chronic disease. Semin Hematol 1983;20(2):61-80.
8. Beutter E. The common anaemias. JAMA 1988;259(16):2433-2437.
9. Means R T, Jr., Krantz S B. Progess in understanding the pathogenesis of the anaemia of chronic disease. Blood 1992;80(7):1639-1647.
10. Means R T, Jr. Advances in anaemia of chronic disease. Int J Hematol 1999;70(1):7-12.
11. Sillness.J,Loe.H Periodontal disease in pregnancy (II). Corelation between oral hygiene and periodontal condition. Acta Odontologica Scandinavica 1964;24:747-759
12. Soskoline W, Kingler A. The relationship between periodontal disease and diabetes. An overreview. Ann Periodontol 2001;6:91-98.
13. Beck J, Offenbacher S. Association between periodontal diseases and cardiovascular diseases: A state of science review. Ann Periodontl 2000;6:9-15.
14. Montebugnoli L, Servidio D, Miaton RA, et al. Poor oral health is associated with coronary heart disease and elevated systemic inflammatory and haemostatic factors. J Clin Periodontol. 2004;31:25-29.
15. Joshipura KJ, Wand HC, Merchant TA, Rimm AB. Periodontal disease and biomarkers related cardiovascular disease. J Dent Res. 2004;83(2):151-155.
16. Aqueda A, Manace C, Guerrero A, Echevemia J. Periodontal disease as a risk factor for adverse pregnancy outcomes; a prospective cohort study. J Clin Periodontol. 2008;35:16-22.
17. Yamamato T, Tsuneishi M, Furuta M. Relationship between disease of erythrocyte count and progression of periodontal disease in rural Japanese population. 2011;82(1):106-113.
18. Nissenson AR, Goodnough LT, Dubois RW. Anemia : Not just an innocent bystander? Arch Inter Med. 163 (12):1400-1404.
19. Lainson PA, Brady PP, Fraleigh CM. Anemia a systemic cause of periodontal disease? J Periodontal 1968;39:35-38.
20. Hutter JW, van der Velden U, Varoufaki A, Huffels RA, Hoek FJ, Loos BG. Lower number of erythrocytes and lower levels of haemoglobin in periodontitis patients compared to control subjects. J Clin Periontol 2001;28(10):930-936.
21. Thomas B, Ramesh A, Ritesh k. Relationship between Periodontitis and erythrocyte count. JISP 2006;10:288-291.
22. Harrison’s principles of internal medicine. 17th ed./editors, Anthony S. Fauci,et al.
23. Wakai K, Kawamura T, Umemura O, Hara Y,Machida J, Anno J. et al: Association of medical status and physical fitness with periodontal disease. J Clin Periodontol 1999;26:664-672.
24. Aljohani HA. Association between haemoglobin level and severity of chronic periodontitis. JKAU: Med Sci, Vol 17 No. 1,53-64.
25. Havemose-Poulsen A, Westergaard J,Stoltze K, Skjodt H, Danneskiod – Sameose B, Locht H, Beneltzen K. Periodontol and haematological charecteristics associated with aggressive periodontitis, juvenile idiopathic arthritis and Rhematoid arthritis. J Periodontol. 2006;77(2):280-288.
26. Enhos S, Duran J, Erden S, Buyukbas S. Relationship between Iron deficiency anemia and periodontal status in female patient. J Periodontol 2009;80:1750-1754.
27. Gokhale SR, Surmanth S, Pandhay AM. Evaluation of blood parameters in patients with chronic periodontitis for signs of anaemia. J Periodontol 2010;81:1202-1206.
|
|
|
|
|
|
|